
Understanding Brain Hematomas: Subdural vs. Epidural
Published on / Category: Car Accidents, Personal Injuries
A blow to the head can change everything. One moment, you’re disoriented—then suddenly, you’re in an ER facing a serious brain injury. When doctors mention a subdural or epidural hematoma, it’s more than just complex terminology. It’s a critical diagnosis that demands fast action.
Understanding the difference between these two injuries isn’t just helpful—it can be life-saving. The type of hematoma affects how quickly treatment is needed, what recovery looks like, and whether legal action may be possible.
You might be here after an accident. Or perhaps you’re trying to understand what went wrong with a diagnosis. Maybe someone you care about is in recovery, and you’re overwhelmed by medical terms and uncertain outcomes.
Whatever brought you here, this guide will help. We’ll explain what subdural and epidural hematomas are, how they differ, how they’re diagnosed and treated—and what legal options exist if someone else’s actions contributed to the injury.

The Brain’s Protective Layers
To understand subdural and epidural hematomas, it helps to know how the brain is protected. The brain is wrapped in three thin layers of tissue called the meninges. These layers cushion the brain, prevent infection, and help absorb impact from trauma.
The Three Meningeal Layers:
- Dura Mater – The thick, outermost layer. It sits just beneath the skull and offers strong structural protection.
- Arachnoid Mater – The web-like middle layer. It supports cerebrospinal fluid flow and cushions the brain.
- Pia Mater – The thin, delicate inner layer. It closely hugs the brain and spinal cord, following every fold and contour.
Bleeding can occur between these layers when the head is struck or jolted.
- A subdural hematoma forms between the dura and arachnoid mater.
- An epidural hematoma occurs between the skull and the dura mater.
Knowing where these bleeds occur is key to understanding how they affect the brain—and how urgent treatment needs to be.
What is a subdural hematoma?
A subdural hematoma occurs when blood collects between the dura mater (the brain’s tough outer layer) and the arachnoid mater (the middle layer). It’s most often caused by a tear in the bridging veins due to head trauma. Common causes include:
- Falls, especially among older adults
- Motor vehicle or bicycle collisions
- Contact sports injuries
- Assault or abuse
The bleeding puts pressure on the brain, which can become life-threatening without quick intervention. Subdural hematomas can form suddenly (acute) or build up over time (chronic). Symptoms vary but may include:
- Severe or persistent headaches
- Confusion, memory loss, or disorientation
- Dizziness, nausea, or slurred speech
- Vision problems or weakness, typically on one side
- Seizures, breathing issues, or unconsciousness in extreme cases
Sometimes the symptoms don’t appear right away—a delay known as a lucid interval. This can make diagnosis difficult and delay treatment.
In some cases, a subdural hematoma may also cause hearing loss or ringing in the ears. If that happens, you may benefit from legal insights on hearing impairments resulting from traumatic brain injuries.
If you or someone else shows signs of a subdural hematoma after a head injury, get medical help immediately. Time is critical.

What is an epidural hematoma?
An epidural hematoma (EDH) is a life-threatening buildup of blood between the skull and the dura mater—the brain’s tough outer covering.
It usually occurs after a skull fracture tears a blood vessel, most often the middle meningeal artery. This arterial bleed rapidly increases pressure inside the skull, putting the brain at risk.
Epidural hematomas are typically caused by:
- Motor vehicle crashes
- Falls
- Blows to the head during sports or physical altercations
Less commonly, they can also result from clotting disorders, infections, or vascular abnormalities.
While not everyone follows the same pattern, many cases begin with a brief loss of consciousness, followed by a lucid interval where the person seems fine. This is often followed by a sudden decline in condition.
Key signs of an epidural hematoma include:
- Intense headache
- Nausea and vomiting
- Drowsiness or confusion
- Slurred speech
- One-sided weakness
- Enlarged pupil on one side
- Seizures or breathing difficulty in severe cases
Why Time Matters
Unlike some subdural hematomas, epidural bleeds usually progress rapidly. If left untreated, they can lead to permanent brain damage or death.
Immediate surgery, often a craniotomy to remove the clot and stop the bleeding, is usually required. This is a true emergency, and the outcome depends heavily on how quickly the hematoma is identified and treated.
Subdural vs. Epidural
While both subdural and epidural hematomas involve bleeding around the brain, they differ in location, cause, progression, and urgency. These differences affect diagnosis, treatment, and legal interpretation—especially in cases involving delayed care or missed warning signs.
Here’s a quick-reference comparison:
Subdural vs. Epidural Hematomas: Key Differences |
||
|---|---|---|
|
Category |
Subdural Hematoma |
Epidural Hematoma |
|
Location |
Between the Dura Mater and Arachnoid Mater |
Between the Skull and Dura Mater |
|
Cause |
Tearing of Bridging Veins, Often Due to Blunt Trauma |
Ruptured Artery (Often Middle Meningeal) |
|
Typical Age Group |
Older Adults, Those on Blood Thinners |
Younger Adults After High-Impact Trauma |
|
Onset of Symptoms |
Delayed—May Take Hours or Weeks |
Often Includes Lucid Interval, Then Rapid Decline |
|
Imaging Shape |
Crescent-Shaped on CT Scan |
Lens (Biconvex)-Shaped on CT Scan |
|
Urgency |
Can Be Acute or Chronic; Always Potentially Serious |
Usually Acute and Immediately Life-Threatening |
|
Common Treatment |
Observation, Burr Hole Drainage, Craniotomy |
Emergency Craniotomy to Relieve Pressure |
These distinctions aren’t just medical—they carry legal consequences. Misdiagnosis, delayed treatment, or failure to act on red flags can dramatically worsen outcomes. Knowing the signs and understanding the differences can help protect both your health and your rights.
Which is more dangerous: subdural or epidural hematoma?
Epidural hematomas are often considered more dangerous in the short term. They usually involve arterial bleeding, which can build pressure rapidly and cause life-threatening brain damage without prompt surgical treatment.
Subdural hematomas, while potentially slower to develop, carry long-term risks. They may go unnoticed for days or even weeks—especially in older adults or those on blood thinners—making them harder to diagnose and treat before complications arise.
In legal contexts, subdural hematomas often raise more complex questions. Because their symptoms may be subtle, proving negligence, delayed diagnosis, or failure to act often requires detailed medical evidence and expert testimony.
Legal Implications of Subdural and Epidural Hematomas
When a brain bleed results from an accident—such as a vehicle collision, fall, sports injury, or medical error—the consequences can be devastating. In many cases, the injury could have been prevented with proper care or timely action.
Proving Negligence or Medical Malpractice
If the injury stemmed from someone else’s actions—like a reckless driver or a negligent property owner—you may have grounds for a personal injury claim. Alternatively, if a healthcare provider failed to diagnose the hematoma, ignored symptoms, or delayed treatment, it may fall under medical malpractice.
In both cases, the core legal issue is the same: Did someone fail to meet a reasonable standard of care?
Your Legal Rights as a Patient
Victims of traumatic brain injuries are entitled to pursue justice. That may include:
- Medical expense reimbursement and coverage for future care
- Compensation for lost wages and reduced earning ability
- Damages for pain, suffering, and diminished quality of life
- Legal accountability for negligent parties
How a Lawyer Can Help
Recovering from a brain injury is hard enough. Navigating a legal battle on top of that can feel overwhelming. That’s why you need comprehensive legal support for brain injury cases.
At Prestige Law Firm, our trusted Palmdale catastrophic injury attorneys help clients:
- Understand their rights and legal options
- Build strong claims supported by expert medical evidence
- Negotiate with insurers and file lawsuits when necessary
We aim to hold the right people accountable—so you can focus on recovery, not red tape.
What compensation is available in epidural or subdural hematoma lawsuits?
A traumatic brain injury doesn’t just affect your health—it can disrupt your job, finances, and entire way of life. If your subdural or epidural hematoma was caused by negligence or delayed medical care, you may be entitled to compensation that helps you recover physically, emotionally, and financially.
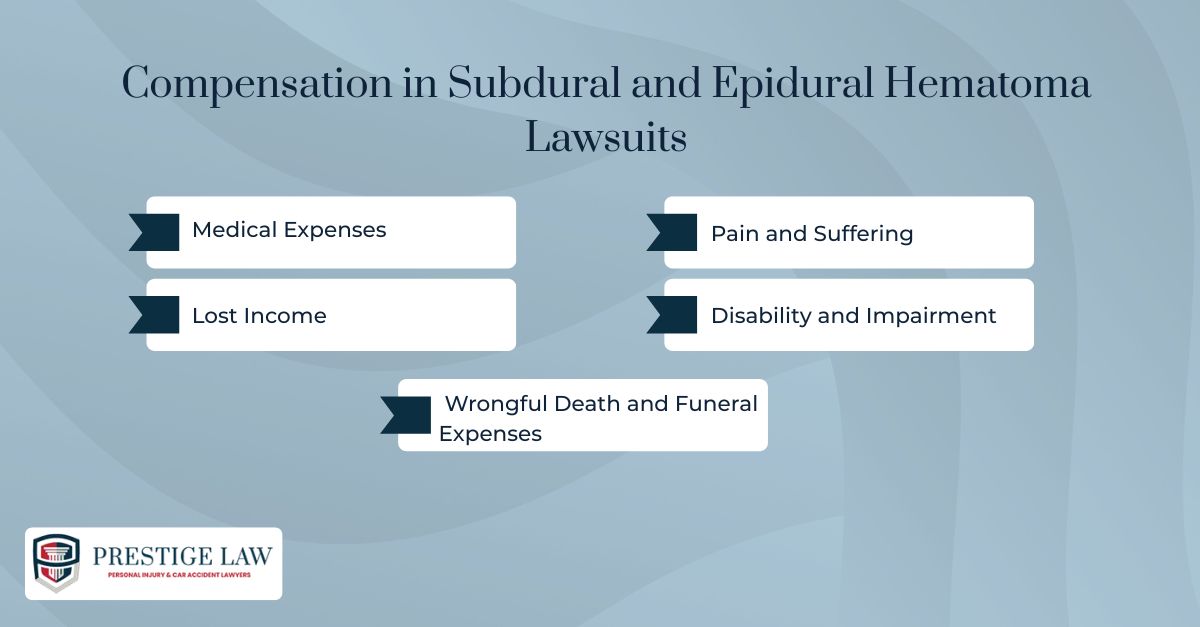
Medical Expenses
This includes emergency care, surgery (like craniotomy or burr hole drainage), rehabilitation, follow-ups, prescriptions, and long-term treatment. Home modifications or adaptive equipment may also be covered.
Lost Income
If the injury prevented you from working—or reduced your future earning ability—you can claim current and projected lost wages.
Pain and Suffering
Compensation for physical pain, emotional trauma, anxiety, depression, and the overall impact on your quality of life.
Disability and Impairment
If the injury results in long-term cognitive or physical limitations, you may be compensated for permanent disability, reduced independence, and need for ongoing assistance.
Wrongful Death and Funeral Expenses
If the injury was fatal, surviving family members may seek compensation for funeral costs, emotional loss, and lost future income.
What Affects the Compensation Amount
Every case is different. The value of your claim depends on:
- Severity and permanence of the injury
- Medical documentation and treatment timeline
- Evidence of lost income and life impact
- The quality of legal and expert testimony
At Prestige Law Firm, we work closely with clients and medical professionals to secure the maximum compensation possible. That way, you can focus on healing while we handle the fight for justice.
What evidence is needed for a subdural or epidural hematoma lawsuit?
A successful hematoma-related lawsuit depends on strong, well-documented evidence. Whether the case involves negligence, delayed diagnosis, or medical malpractice, your claim must clearly show fault, injury severity, and resulting damages.
Here’s what typically strengthens a brain hematoma case:
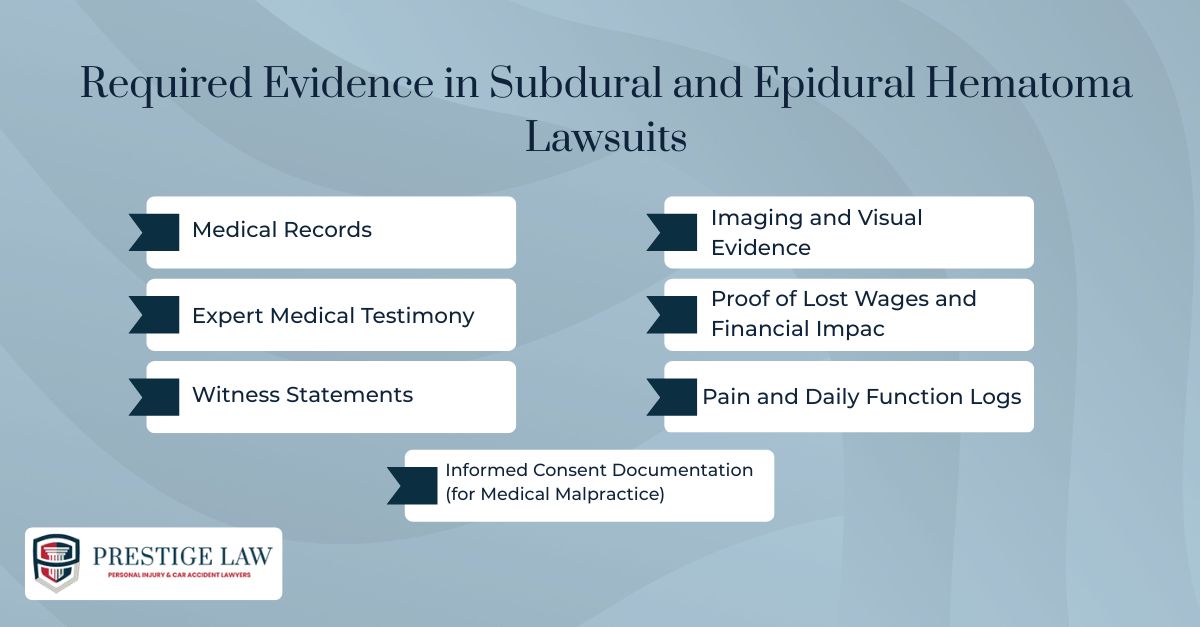
Medical Records
These are the foundation of your case. You’ll need:
- CT scans or MRIs showing the hematoma
- ER intake and discharge summaries
- Surgical notes (e.g., craniotomy, burr hole)
- Ongoing neurological assessments and rehab records
Expert Medical Testimony
A qualified physician (often a neurosurgeon or ER doctor) can:
- Explain standard-of-care expectations
- Identify how those standards were breached
- Link the breach to your injuries
Witness Statements
Statements from anyone who saw the incident or has observed your symptoms (family, coworkers, medical personnel) add weight to your narrative and show how the injury has changed your life.
Imaging and Visual Evidence
High-resolution images of the hematoma (from CT or MRI scans) serve as visual confirmation. Photos of external injuries or recovery milestones can further document your journey.
Proof of Lost Wages and Financial Impact
Gather:
- Pay stubs, W-2s, or tax returns
- Employer statements on missed work
- Future income projections (if the injury causes long-term disability)
Pain and Daily Function Logs
Personal journals tracking your pain levels, sleep issues, medication side effects, and emotional distress are valuable in demonstrating non-economic losses like suffering and reduced quality of life.
Informed Consent Documentation (for Medical Malpractice)
If your case involves a failed procedure (like an improperly performed epidural), documentation showing whether you were fully informed of risks before treatment can be pivotal.
Conclusion
A subdural or epidural hematoma is more than just a diagnosis. It’s a medical crisis that can alter your health, career, and entire future.
If the injury was caused by a fall, collision, or a delayed diagnosis, the question becomes: Who’s being held responsible? Who ensures you’re not left managing the consequences alone?
At Prestige Law Firm P.C., we’re here to guide you through that process. With over two decades of experience and a focus on traumatic brain injury cases, our team includes experienced attorneys for catastrophic injury claims who know how to fight for the justice you deserve.
Read client experiences with our brain injury legal services to understand how we’ve helped others in similar situations.
Whether your case involves a catastrophic injury from a vehicle crash, a failed medical response, or a workplace accident, we’ll help you secure the care, compensation, and justice you deserve.
📞 Call (818) 788-0808 or (661) 341-3939 to speak with a live agent 24/7
🌐 Visit: prestigelaw.com
FAQs
How are subdural and epidural hematomas diagnosed?
They are diagnosed using brain imaging tests—typically a CT scan or MRI—after symptoms arise or following a head injury. These tests help determine the bleed’s location, size, and urgency.
What are the treatment options for these types of hematomas?
Treatment depends on severity. Smaller bleeds may only require observation. More serious cases often need surgery, such as burr hole drainage or a craniotomy, to relieve pressure and prevent brain damage.
Can you recover fully from a subdural or epidural hematoma?
Yes, many people recover completely, especially with prompt treatment. Recovery depends on factors like the size of the bleed, the speed of diagnosis, patient age, and overall health.
Get Started Today!
24 hours a day / 7 days a week / 365 days a year
Contact our Los Angeles attorneys for a free consultation today
